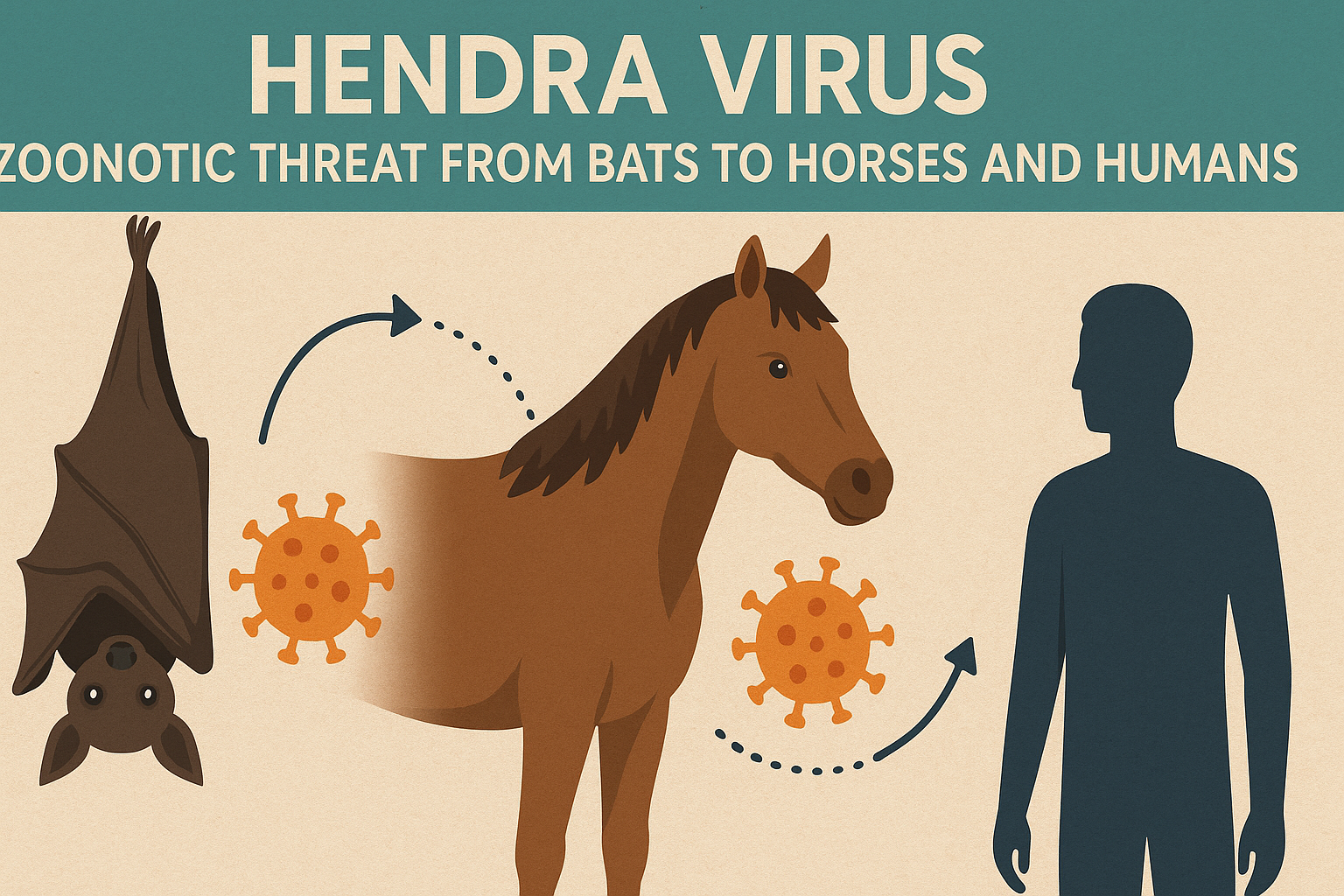
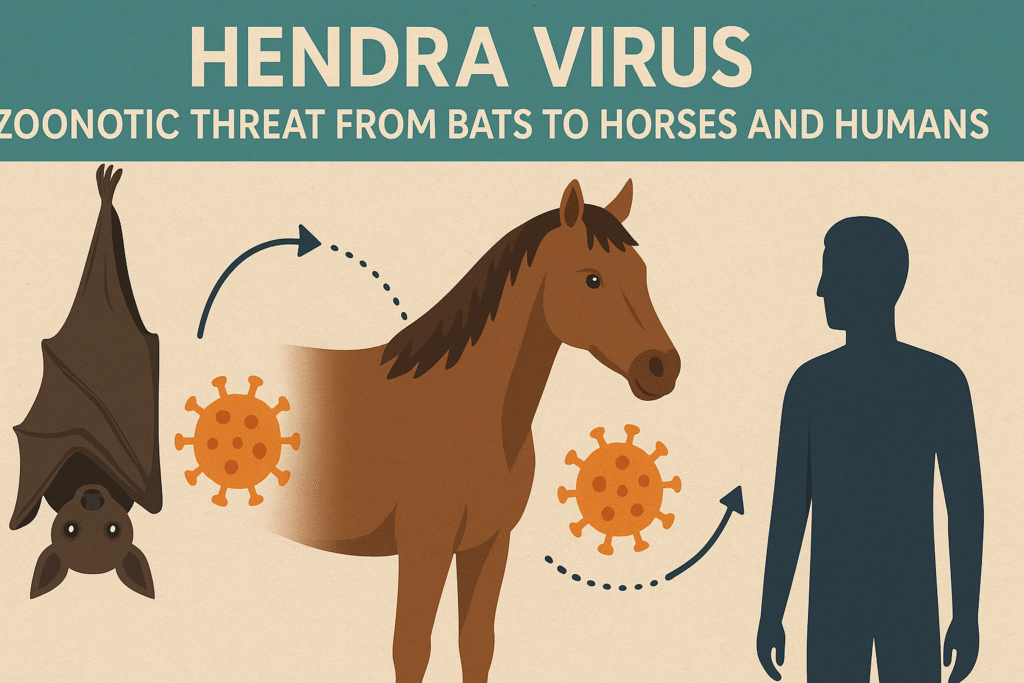
Hendra virus (HeV) is a rare but highly pathogenic zoonotic virus first identified in 1994 in Hendra, a suburb of Brisbane, Australia. Belonging to the genus Henipavirus within the Paramyxoviridae family, it is closely related to the Nipah virus and poses a significant public health concern due to its ability to transmit from animals to humans, causing severe and often fatal disease.
The virus’s natural reservoir is fruit bats of the Pteropus genus, commonly known as flying foxes, and it primarily affects horses, with occasional spillover to humans. This article explores the epidemiology, transmission, clinical manifestations, diagnosis, prevention, and ongoing research surrounding Hendra virus, emphasizing its impact and the measures to mitigate its risks.
Epidemiology and Emergence
Hendra virus emerged in September 1994 during an outbreak in a racing stable in Hendra, Brisbane, where it caused the deaths of 14 horses and one human, a horse trainer. Since then, over 60 incidents involving more than 80 horses have been reported, primarily along Australia’s northeastern coast, particularly in Queensland and northern New South Wales.
Seven human cases have been documented, with four fatalities, yielding a human case-fatality rate of approximately 57%. The virus’s sporadic outbreaks, often linked to environmental and ecological factors, highlight its unpredictability and potential for severe outcomes.
The reservoir hosts, flying foxes, are widespread in Australia, with a seroprevalence of 47% indicating endemic infection. The virus does not cause illness in bats but is shed in their urine, feces, and saliva, facilitating transmission to horses. Outbreaks have been associated with habitat loss and climate variability, which drive bats into closer contact with horses due to food shortages.
For instance, nectar scarcity can lead bats to roost near equine habitats, increasing spillover risks. A notable increase in cases occurred in 2011, with 23 incidents, underscoring the influence of environmental stressors.
Transmission
Hendra virus is primarily transmitted from flying foxes to horses through contact with contaminated bodily fluids, such as urine or saliva on pasture or feed. Horses act as amplifying hosts, developing high viral loads that can infect humans through close contact with their respiratory secretions, blood, or other fluids. Transmission typically occurs during the care or necropsy of infected horses, as seen in cases where veterinarians or handlers were exposed without adequate protective equipment.
Horse-to-horse transmission is rare and requires close contact, often in confined settings like stables. No human-to-human transmission has been documented, reducing the risk of widespread outbreaks but not eliminating the danger to those in direct contact with infected horses.
Clinical Manifestations
In horses, Hendra virus causes a range of symptoms, from mild to severe, with a fatality rate of about 75%. Early signs include depression, inappetence, and mild respiratory or colic-like symptoms.
As the disease progresses, horses may exhibit fever, elevated heart rate, respiratory distress, frothy nasal discharge, ataxia, or neurological signs such as head pressing or disorientation. Terminally ill horses often succumb to pulmonary edema or neurological complications.
In humans, the incubation period ranges from 5 to 21 days, with symptoms varying from mild influenza-like illness to severe respiratory or neurological disease. Initial signs include fever, headache, myalgia, and cough, which can escalate to pneumonia, respiratory failure, or neurological conditions like encephalitis or meningitis.
Of the seven human cases, four were fatal, often due to severe respiratory or neurological complications. The high case-fatality rate underscores the virus’s lethality, though its rarity limits widespread impact.
Diagnosis
Diagnosing Hendra virus involves detecting viral RNA or antibodies in affected horses or humans. Quantitative real-time reverse transcriptase polymerase chain reaction (qRT-PCR) assays on blood, urine, nasal, or oropharyngeal swabs are the primary diagnostic tools, with results typically available within 24–48 hours.
Serological tests, such as enzyme-linked immunosorbent assay (ELISA), screen for antibodies, while virus neutralization tests confirm infection. In Australia, testing is conducted at facilities like the CSIRO Australian Animal Health Laboratory in Geelong.
Early sampling may yield false negatives, necessitating repeat tests. Veterinary professionals must conduct risk assessments and use strict biosecurity protocols when handling suspected cases due to the virus’s Biosafety Level 4 classification.
Prevention and Control
The most effective preventive measure is the Equivac HeV vaccine, a subunit vaccine targeting the virus’s G glycoprotein, fully registered in Australia since 2015. Over 300,000 doses have been administered, significantly reducing equine infections and human exposure risks.
The vaccine, safe for pregnant mares, has minimal side effects, primarily localized swelling. Other preventive strategies include relocating horse feed and water containers away from trees frequented by flying foxes and implementing strict biosecurity protocols, such as using personal protective equipment (PPE) and maintaining hygiene among horse handlers.
Environmental management is also critical. Reforestation efforts to restore bat feeding grounds can reduce their proximity to equine habitats, lowering spillover risks. Public health campaigns emphasize vigilance, urging veterinarians and horse owners to report suspected cases promptly to authorities, such as Australia’s emergency animal disease hotline (1-800-675-888).
Treatment and Research
No specific antiviral treatments exist for Hendra virus in humans or horses. Supportive care, including intensive respiratory and neurological management, is the mainstay of treatment. Research into monoclonal antibodies targeting the virus’s G glycoprotein is ongoing, with promising results in animal models, but no licensed therapeutics are available for humans.
The Equivac HeV vaccine remains the primary tool for reducing transmission. Studies are also exploring point-of-care diagnostics and the role of inflammasomes, such as NLRP3, in driving inflammation, which could lead to novel therapeutic targets.
Ecological and Climate Impacts
Climate change and habitat loss exacerbate Hendra virus spillover. Deforestation and nectar shortages force flying foxes into urban or peri-urban areas, increasing contact with horses.
Research indicates a correlation between bat nutritional stress and higher viral shedding, particularly during breeding seasons. Addressing these ecological drivers requires a One Health approach, integrating human, animal, and environmental health strategies to mitigate zoonotic risks.
Conclusion
Hendra virus remains a significant zoonotic threat due to its high fatality rates and potential for spillover from flying foxes to horses and humans. While rare, its impact on equine industries and public health necessitates robust preventive measures, including vaccination, biosecurity, and ecological management.
Ongoing research into diagnostics, therapeutics, and ecological drivers is crucial to reducing the virus’s threat. By combining scientific advancements with proactive environmental strategies, Australia continues to lead efforts in controlling this deadly pathogen, offering a model for managing emerging zoonotic diseases globally.